By Ellen Mortensen-The Gothenburg Leader
93 days and counting for Alan and Jenny Daup
No one goes through a difficult time - loss, hardship, disease - alone. When someone we love hurts, we hurt. Alan Daup’s journey began three months ago. And his loving family has been there every step of the way.
The medical world is far from an unfamiliar place for Alan. He holds a bachelor of science degree in occupational therapy from Creighton University, and a master’s degree in business administration from the University of Colorado at Colorado Springs. At the time this began, he was employed as an occupational therapist at Gothenburg Health.
Alan was in Omaha helping his daughter, Maddie, with some projects that needed to be done on the house that she lives in. On Jan. 5, he woke up with terrible cramps in his stomach and a high fever. “There was a stomach virus going around at Christmas time and he thought that he probably had that,” his wife Jenny explained. “Maddie called me and thought Alan should go to the ER but he thought he just had a virus. I came to Omaha that night to take him back home and get the virus out of Maddie’s house, but he was too nauseous for me to drive him home.”
Jenny said the next day Alan was not as nauseous but his fever was still high. “We thought this was progress so we just let him sleep off and on all day. When he woke up on the 7th and was not any better, we decided to go to the ER at Creighton University/Bergan Mercy Hospital. At first, the doctors thought he just had gastroenteritis but they did a CT scan and within 15 minutes, they had a surgeon talking to us and were preparing him for emergency surgery,” she said. “There happened to be a vascular surgeon at the hospital that day who had just finished another surgery. They had two different surgeons doing surgery that first day- a general surgeon to take care of the intestines and a vascular surgeon to patch the hole in his superior mesenteric artery and to clear out the clot in that artery.”
There was a hole in the artery and as the body tried to heal itself, it formed a clot in the artery, Jenny explained. The clot had completely cut off the blood supply to his small intestine. A second surgery was performed the next morning which was exploratory surgery to confirm that the intestines were still healthy.
“They thought that the intestines were probably going to have some ischemic (dead) spots that would need to be removed because he had spent 50 hours in this condition before he had the surgery,” said Jenny.
With the complications of such a major surgery entailing the digestive system, it was two full weeks before Alan was reintroduced to solid food. On Jan. 21 he was given the green light to eat anything he wanted. He started small - just some fruit - but became nauseous after only three bites. His intestines had still not “woke up” to begin processing food again yet, so they waited.
In the meantime, a central line had been inserted to provide “feeding” directly into his stomach, commonly known as an NG tube. However, Alan had encountered some pretty serious complications along the way, including a collapsed lung.
“After a week or two, Alan had some unexplained bleeding in his digestive tract and they thought they were going to have to do a colonoscopy so they stopped his heparin (a blood-thinning medicine) to be able to safely do the colonoscopy,” explained Jenny. “When they stopped that medicine, the bleeding in his digestive tract stopped so they did not have to do anything...but the clot re-formed in the superior mesenteric artery at that time. The blockage came back and the doctors were just shocked and terribly concerned.”
On the evening of Jan. 24, things took a severe turn for Alan. “Alan became septic and the critical care team earned their gold stars,” Jenny shared. “He was stable but the sickest we had seen him. We were so very thankful that he made it through the night. He was intubated and hooked to every tube and machine known to man.”
He was placed on a ventilator, but luckily that was very short term. By late morning on Jan. 26, the vent had been removed and Alan was talking, laughing and joking with his family and team of nurses. A new drain tube was inserted to remove the infected fluid from his body, and things were looking up. On Jan. 30, he went for his first walk in a week, and his white blood cell count was nearly back to normal - which meant the antibiotics and drainage tube were working. He was also able to have the NG tube removed.
Doctors were uncertain, however, about the clot. “The doctors didn’t think it was gone but were hopeful that the intestines might have enough blood flow from the smaller vessels to work, regardless of the status of the clot,” Jenny explained.
Once again, just as Alan seemed to be taking steps forward he would take more steps back. A CT scan on Feb. 3 revealed he had multiple small perforations in his bowel which were leaking into his abdomen. “They were likely due to all of the swelling that happened throughout all of this - nothing anybody did wrong - just what happens when tissue is swollen and irritated for a long period of time,” said Jenny.
He was scheduled for surgery later that day, and doctors anticipated at least another 10 days in the hospital following that. In the meantime, they discovered the blood clot had not dissolved, but the small blood vessels had stretched to compensate for the artery and were supplying the blood flow Alan needed for his small intestine to stay healthy. Good news.
“I have done a LOT of reading about this darn clot that started this whole adventure,” said Jenny. “Since it re-formed, I wanted to understand everything I could about why this might have happened and what the future might hold. It is still a mystery. It is very rare for a clot like this to spontaneously occur. God put us in the right place at the right time to allow Alan to survive. The survival rate for this is 50% when it is discovered and surgery performed in the first 24 hours after it has occurred. The survival rate drops to 30% after the first 24 hours. Alan’s clot was not even discovered until 55 hours after he had his first symptoms.”
The surgery to repair the perforations in his bowel was a success. A section of his small intestine was removed but he was expected to make a full recovery. However, a few days later he was still unable to speak out loud and had to resort to whispering and writing on a board to communicate. An ENT specialist concluded that Alan had sustained some nerve damage from being intubated which caused vocal cord paralysis. Though the timeframe was uncertain, the doctor did expect the issue to resolve on its own.
Unfortunately, the paralyzed vocal cord did not just affect his ability to speak. “It turns out that your vocal cords tighten together to cover the opening into your lungs when you swallow,” Jenny explained. “They found that all liquid and food (thick or thin) was going right down into his lungs. So, that means he could not eat or drink until that paralysis is over - which did not have any time frame.”
Alan and Jenny had a big Valentine’s Day celebration when a swallow study resulted in his being able to eat solid foods and drink thickened liquids once again. “I went a little crazy with a variety of tastes for him,” Jenny laughed.
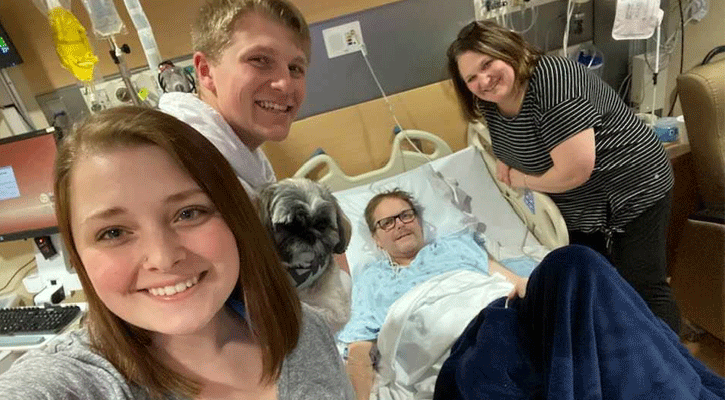
Meanwhile, life went on around them. The couple’s two children, Maddie and Seth, continued to have activities and school events that their dad was not able to be there for. But thanks to modern technology he wasn’t missing everything - Alan got to watch Seth’s confirmation in real-time over the Internet.
Feb. 19 was a good day for Alan. He slept well, ate some food, took a couple of walks and had a good session with the speech-language pathologist who was encouraged that the whisper was getting stronger and louder. But on Feb. 25, he began experiencing abdominal pain that became unbearable. Another CT scan revealed Alan had a bowel obstruction and the team began preparing for surgery the following day. What happened next, Jenny will tell you, was nothing short of a miracle.
“We started the morning with the plan for Alan to have surgery to remove a bowel obstruction. Right before they went in for surgery the doctors sat me down to deliver the news that Alan’s scans showed more than a bowel obstruction - they showed that he had an ischemic bowel, an obstruction and a likely perforation. His lactic acid levels had gone up significantly overnight. The doctors wanted me to be aware that they believed he was beginning to become septic and they wanted me to be prepared for any of a number of outcomes to this. They believed that his bowel was probably not healthy and they were sure that they would be removing at least part of it.
“Their theory was that the lack of blood flow from the clot was slowly taking a toll on the bowel and parts of it were likely dying off,” Jenny continued. “They warned us that removing a portion would stabilize him enough for us to make some decisions about how far we wanted to go - that it was possible that this would happen over and over again until he no longer had enough intestine to process nutrition. There was a possibility that he would leave the surgery with an ostomy bag. Then came the miracle.
“Dr. Sasse came into the consultation room and the first thing she told us was, ‘I did not expect to see what I saw when we first opened him up. I expected his intestines to be in bad shape but they were pink. They were not swollen and they did not look bad at all. The reason that it took us so long in there was that we explored every inch of them and we could not find a single thing wrong with them. We didn’t find any holes, we didn’t find a blockage, and when we looked at the place that we repaired before, we found that it was completely fused - so well that you can barely see the stitches. We don’t know why his labs looked bad this morning. Maybe he is getting a touch of pneumonia or maybe it is because we were flushing his drainage tubes for the past couple days because they had stopped draining and that irritated things a little bit - but we don’t have an explanation for what we found.’”
His insides did not look anything like what the scans showed. In fact, she said that his intestines looked BETTER than the last time they finished surgery.
Within 48 hours of the surgery, Alan’s pain was under control, he was awake and alert and cracking jokes. The next turn would come just a couple of days later. Alan’s surgical wound was in really bad shape, and for two weeks Jenny had been asking for a referral to the wound team. The surgeons finally agreed; the wound care team put a plan in place and went right to work.
On March 20, two weeks after beginning the wound care, Alan had skin graft surgery which took a section of skin from his leg to be grafted onto his belly. The official “reveal” of the skin graft came on March 26.
“Initially, the surgeons wanted to wait five days before peeking at the skin graft, but they had to change some dressings early. Their early glimpses had them fairly sure that the graft was doing ok and when they took a good look at it they were happy to report that it was successful! We thank God that through all of the issues - Alan’s skin graft has remained healthy and he won’t have to have a second one,” Jenny said. The first plan was for a small graft, wait five days, then a second small graft, and wait five more days.
While the doctors had great success with the skin graft, they were struggling to get Alan’s digestive system to heal. They believed that was likely due to the clot which remained in the main artery in his abdomen. But there is progress. On April 1, Alan was moved to a real bed and was able to stand up for the first time in three weeks. The skin graft is healing well.
And then there’s COVID-19. The hospital has taken the steps of closing to most visitors, and on Tuesday night, March 31, Maddie and Seth got to spend the last evening with their dad until this ordeal is over. Jenny was granted an exception and gets to remain with Alan in their new “home-away-from-home”.
“I won’t be allowed to leave at all. We are so grateful for this little mercy which will allow me to be with him,” Jenny said. “His situation is so complex and changes so quickly that I cannot begin to tell you how much of a relief it is to be able to stay with Alan.”
His extended hospital stay has dealt the couple another blow as well. They were notified that as of April 7, Alan will have been absent from work for 90 days - and since the company does not meet the requirement to offer FMLA, his employment was terminated at that time.
“I completely understand that they have a policy that they have to follow for everyone,” said Jenny, noting that this is just an unfortunate circumstance. “They assured me they will welcome him back when he is able to return to work. We have had wonderful support.”
Because the family’s health insurance is provided through Alan’s employment, Jenny has been busy finding an alternate resource. Though very expensive, she said they will be able to have COBRA insurance for 18 months.
For now, they are hunkered down at Bergan Mercy Hospital - waiting, healing, and thanking God every day for his continued blessings.
Contact Ellen Mortensen at [email protected] or call 308.536.6499




