Editor’s Note: The following story is based on the personal accounts of Janeen White Gill’s daughters, including Anastasia and Autumn Miller, and social media posts shared publicly. Allegations referenced in this story are not the same as confirmed disciplinary actions, and under U.S. law, individuals are considered innocent until proven guilty. The family has removed the nurse's name from their post to avoid diverting attention from what they feel is the main focus. Nebraska’s licensing website shows that Luci Duggan’s nursing license remains active. It's important to note that while these accounts are emotionally charged, Great Plains Health is bound by HIPAA privacy laws and cannot confirm or deny any allegations detailed.

A Year Without Janeen
One year has passed since the sudden death of Janeen White Gill, a 50-year-old mother, grandmother, and mental health therapist from North Platte. Her daughters say their grief remains matched by anger — not only over the medical events they say led to her passing but also over the way they feel she was treated in her final days and even after her death.
“This is our family’s story,” wrote Anastasia Miller in a Facebook post calling for accountability. “It’s a story of unimaginable loss, medical negligence, and the total lack of dignity shown to our mother. Not just in her final days, but even after her death.”
The Timeline of a Hospital Stay
On the night of September 22, 2024, Janeen went to the emergency room at Great Plains Health (GPH) in North Platte, suffering from severe abdominal pain. Doctors determined she had a twisted colon, a condition known as volvulus, and she underwent emergency surgery performed by a traveling surgeon.
Anastasia said her mother was transferred to the ICU, where she spent several days in pain. According to her daughters, Janeen repeatedly complained of extreme discomfort, yet no abdominal CT scan was performed in the days following the operation.
By the morning of September 26, doctors discovered that Janeen had suffered a gastrointestinal perforation — a hole in the stomach that can quickly become life-threatening. She was rushed, said Anastasia, into another emergency surgery. Afterward, doctors placed a wound vac and put her on a ventilator to rest.
That evening, the family stated they received a phone call from a nurse. Janeen’s blood pressure was low, and her scheduled procedure to remove the wound vac and close her abdomen was postponed. The nurse told them Janeen was no longer sedated but that “her body was putting itself into a coma so that it could heal.”
Through the night into the morning of September 27, Janeen developed hyperpyrexia — an extreme fever reaching 107°F. Hyperpyrexia is a medical emergency that can cause irreversible brain damage, organ failure, and death if not treated immediately. According to the family, Janeen endured this fever for more than 12 hours without the urgent intervention they believed was necessary.
By the following day, her organs were failing, and she was in septic shock. Her daughters were told that if she regained consciousness, she would likely lose her limbs due to restricted blood flow. On September 28, 2024, at 9:33 p.m., Janeen died surrounded by her four daughters.
A Breach of Trust
Weeks after Janeen’s death, the family discovered a post in the “NO LIMITS – North Platte, Neb.” Facebook group alleging that an ICU nurse, identified by the family as Luci Duggan, removed Janeen’s wound vac after her death, took photos of her organs, and shared them with others. The post suggested the nurse had been fired.
The family contacted the patient advocate at Great Plains Health, who confirmed that Duggan had committed a "serious HIPAA violation" and apologized. The advocate also indicated that the hospital had attempted to remove the post quickly, suggesting, according to the family, that they did not want the public to see it.
“Sharing images of her body — after she passed, after all she endured — was a violation of basic human decency. Unfortunately for them, I saw it,” Anastasia said.
Nebraska’s licensing website shows that Duggan’s nursing license remains active.
The Life Lost

For her daughters, remembering Janeen is about far more than the circumstances of her death. Her daughters said she was a woman who had just reached milestones that marked both pride and promise.
“We celebrated her 50th birthday in June 2024, months before her life was taken,” Autumn Miller shared. “Also, in July 2024, she earned her doctorate degree, something she had worked so many years for. She spent 5 years writing her dissertation. She walked the stage to receive her doctorate just two weeks before she died.”
Janeen was a practicing mental health therapist in North Platte and had built her own practice. Her daughters describe her as a mother who never missed a moment in their lives, even when it wasn’t easy.
“She was the most amazing mom,” Autumn said. “She supported us 4 girls in whatever we did. She always showed up for us, no matter how inconvenient it was for her.”
Janeen was also stepping into a new chapter of life she had long dreamed of: becoming a grandmother. Her first grandchild was born in 2022, and her second was on the way when she passed.
“My mom never got to hold her grandson,” Autumn said. “A simple look at her Facebook would show you how proud she was of being a grandma. She’ll never get to meet any of her future grandkids. She’ll never get to practice with her doctorate. Not only was she a mother, she was a grandma, a daughter, a sister, an aunt, a niece, a therapist, and so much more to those who knew her. She endured a lot in her life, but she taught us girls to keep going and not back down. She was a warrior. And I’m proud to call her my mom.”
Seeking Accountability
For the Miller family, speaking out is about more than grief — it is about making sure no other family endures what they say they did. They say they want answers, change, and safeguards for patients at Great Plains Health.
Anastasia Miller described the ongoing pain and determination her family feels:
“We are seeking accountability and justice. Our mom was not given the care she deserved, not by any stretch of the imagination. We are heartbroken by the suffering she endured, and we are sickened by the way she was disrespected after she passed.”
She emphasized that their fight is not just personal, but a "warning" to protect others:
“If this could happen to our mom, it could happen to someone else. And if GPH won’t protect its patients, then we will speak until they do.”
Their mission, she says, is about more than justice:
“Our fight isn’t just for justice. It’s for her memory, her dignity, and for every patient who deserves better.”
Great Plains Health Responds
Great Plains Health extended its “deepest sympathy to anyone who has lost a loved one,” acknowledging that the loss of a family member or friend is always difficult.
The hospital emphasized that, due to federal HIPAA privacy laws, it cannot discuss specific cases. It noted that patient privacy is a top priority, with new employees receiving comprehensive HIPAA training and ongoing monthly and quarterly reminders. Any privacy violations are reported to the patient, the Office of Inspector General, and, in severe cases, state licensing authorities, with violations potentially resulting in termination.
Like many hospitals nationwide, Great Plains Health occasionally employs traveling physicians to ensure continuous coverage, particularly during extended vacations or maternity leave. The hospital also highlighted its permanent surgical staff, including four general surgeons, three of whom grew up in the region and are committed to the health of the local community.
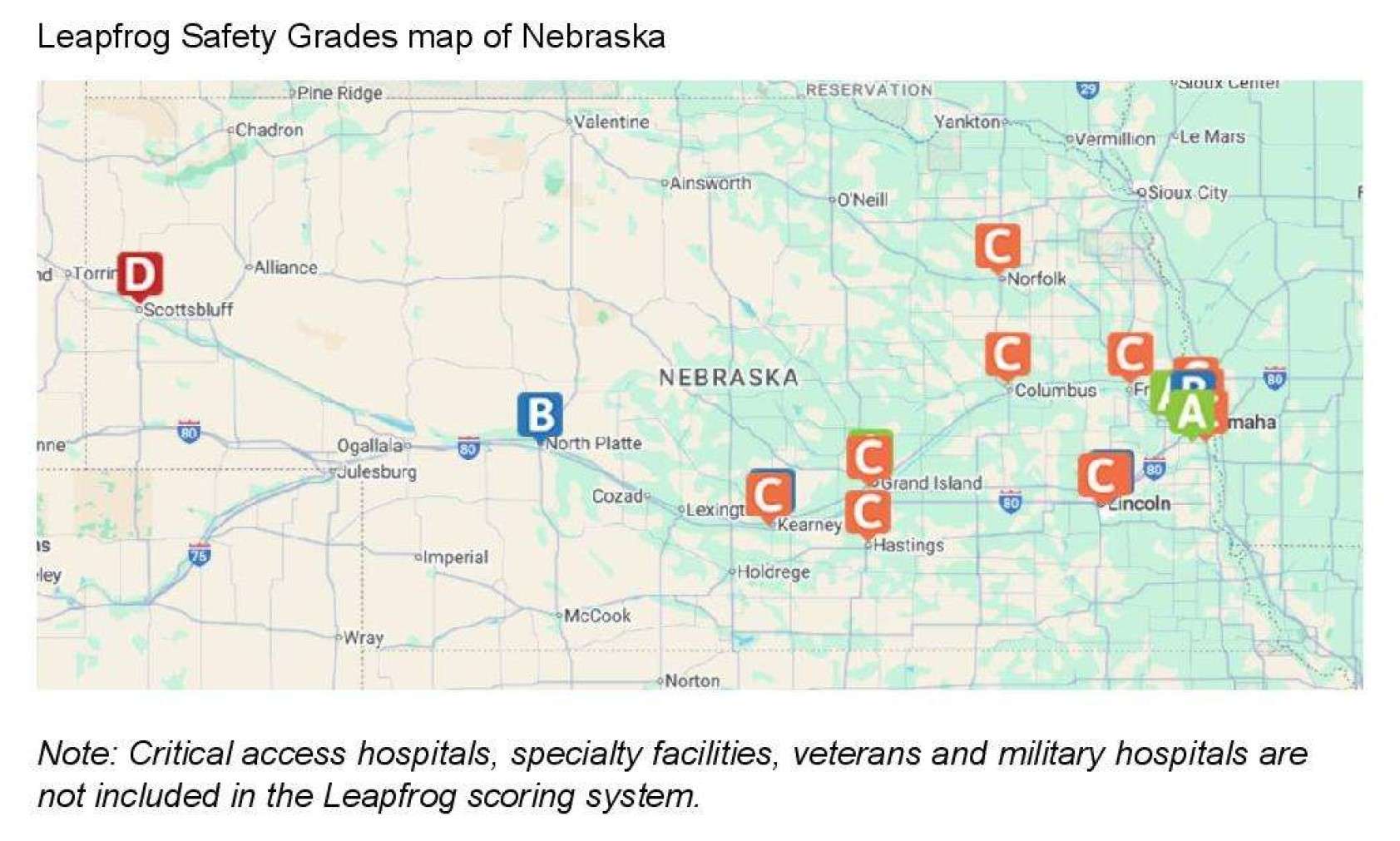
Great Plains Health also highlighted its national patient safety performance. In the most recent Leapfrog Hospital Safety Grade report, the hospital received one of the top scores in Nebraska, with only three hospitals in the state ranking higher. Leapfrog evaluates hospitals on measures such as infection prevention, surgical safety, and staff responsiveness. Additionally, Great Plains Health’s observed-to-expected mortality rate as of August 2025 is 0.58 — meaning the hospital has fewer deaths than expected based on national benchmarks, reflecting performance above the national average.
The statement concluded by noting the challenges inherent in healthcare and acknowledging that perfection is not always possible. “Still, we are proud of the quality of care provided at Great Plains Health and how we compare on a national level. Our community can have confidence in an organization deeply committed to excellence, compassion and the health of the people we serve,” the release read.




